
Garden and Plate
The Molecular Biology of Nutrition











Sweet fructose and the bright red color are marketing gimmicks used by the strawberry plant to persuade animals to consume it and scatter it's seeds. These berries are just one of many ways that carbohydrates enter the animal kingdom.
Carbohydrates enter the animal kingdom when a plant is consumed. Plants create the carbohydrates from carbon dioxide and water, using the power of the sun in a process that's called photosynthesis. They move the carbohydrates throughout the plant, and rearrange the atoms and molecules of the carbohydrates for their own purposes. They use starch for storage, cellulose for structure, sucrose for transport, glucose for energy, and fructose to sweeten their fruit. Animals need carbohydrates as well, but they have to get them from the plants. Animals can't produce carbohydrates from scratch, since they can't do photosynthesis.
Animals have adapted to what the plants have to offer, even though animals and plants don't always have the same needs. Animals can use glucose directly, but must convert fructose into glycogen or fat before it can be broken back down into glucose. Sucrose and starch must be broken down into glucose and/or fructose before it can be absorbed into the body, and cellulose can't be broken down at all. Animals don't use cellulose for structural purposes, since we use bones for support. But after millions of years of having to adapt to cellulose in plant-based foods, our digestive system has adapted to it, and won't function properly without it. We refer to the cellulose in our diet as fiber, and it's now an essential component of our food.
When animals eat plants, they aquire a mixture of carbohydrates that must be processed in a variety of ways, depending on their molecular structure. Glucose, galactose and fructose are monosaccharides (single-sugar molecules), and don't need to be broken down (digested) at all. They are absorbed from the small intestine into the portal vein that leads directly to the liver.
Sucrose, lactose and starch are all handled differently because they need to be broken down into the smaller monosaccharides before they can be absorbed. Sucrose and lactose are disaccharides (double-sugar molecules). Sucrose consists of glucose and fructose that are bound together. This bond must be dissolved by the sucrase enzyme in the small intestine before the glucose and fructose can be absorbed. Lactose consists of glucose and galactose, which must be separated by lactase.
Starch, on the other hand, is a long strand of glucose molecules that doesn't contain any fructose or galactose at all. The breakdown of starch begins in the mouth, where the amylase enzyme gets an early start. Amylase complete's it's job in the small intestine where the starch that wasn't broken down into glucose earlier is finished up. Starch bonds can only be dissolved from the ends of the starch strands, one glucose molecule at a time, so the digestion of starch takes time. That's why candy bars (containing mostly sucrose) give you a quick burst of energy, while pasta (containing mostly starch) gives you a less intense, but longer lasting energy level.
Cellulose is another story. It's composed of glucose units, just like starch, but is bound together into a structural configuration that is unbreakable by the amylase enzyme. While all of the glucose units in starch are oriented in the same position, the glucose units in cellulose alternate their orientation relative to each other. Cellulose leaves the body without having any of it's glucose absorbed, and provides no nutritional value. It does, however, provide bulk that the body needs in order to digest the nutritious components of food properly.
When all is said and done, the only carbohydrates that enter the portal vein from the small intestine are the monosaccharides; glucose, galactose and fructose. The portal vein transports them directly into the liver, where they are handled in very different ways. Galactose and glucose are distributed throughout the body, where they can be used by every cell. Fructose can't be used by most cells, so the liver must deal with all of the fructose itself. These processes all occur inside individual cells, and are part of cellular respiration, not digestion. You can read about them on the pages that discuss glycolysis and fructolysis. The regulation of glucose in the bloodstream, however, is an important part of the digestive process.
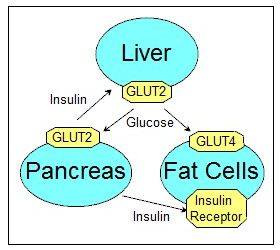
Levels of glucose in the bloodstream (blood-sugar levels) are regulated in a three-way feedback loop between the liver, the pancreas, and the muscle and fat cells. Here's how the balance is maintained.
Glucose is absorbed from the small intestine into the portal vein after you eat a meal. The portal vein then transports it into the liver where it's either converted into glycogen and triglyceride for storage, or allowed to pass unaltered into the bloodstream.
Once in the bloodstream, glucose enters and exits the cells through passageways that are embedded in the cell membranes. The passageways go through proteins called GLUTs (GLUcose Transporters). There are two types of GLUTs that transport glucose. GLUT2 is embedded in the membranes of liver and pancreas cells, while GLUT4 is embedded in the membranes of muscle and adipose (fat) cells. GLUT2 passageways are always open, allowing glucose to freely enter pancreas and liver cells. GLUT4 passageways can be opened or closed by changing the position of the GLUT4 protein in the cell membrane. This is controlled by the pancreas.
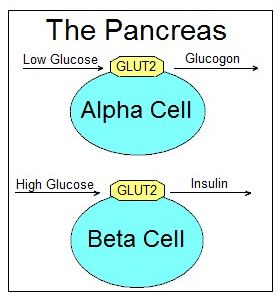
The pancreas regulates glucose levels in the bloodstream by measuring the amount of glucose that enters it's alpha and beta cells through the GLUT2 openings in their membranes. When glucose levels rise too high, the beta cells release a hormone called insulin into the bloodstream. When glucose levels are too low, the alpha cells in the pancreas release a hormone called glucogon.
The released insulin circulates in the bloodstream until it binds to an insulin receptor; a protein that's embedded in the cell membrane of a muscle or fat cell. This causes the phosphorylation of multiple proteins inside the cell, which leads to the repositioning of the GLUT4 protein. This in turn opens a passageway that allows glucose to diffuse into the cell, where the glucose concentrations are lower.
Once inside, the glucose is transformed into glucose 6-phosphate. This not only keeps the glucose from diffusing back out of the cell, but also lowers the amount of unphosphorylated glucose inside the cell, allowing the diffusion of even more glucose into the cell. This process lowers blood-sugar levels until the lack of glucose entering the beta cells in the pancreas causes it to stop producing insulin. The insulin that's already attached to the insulin receptors degrades over time, causing the GLUT4 openings on the muscle and fat cells to close. Muscle cells use the imported glucose right away for energy, or store it as glycogen for later use. Adipose cells store the imported glucose they don't need as triglycerides (fat).
Insulin also reduces the amount of glucose that enters the bloodstream from the liver. It does this by dephosphorylating two enzymes. It activates glycogen synthase, which stores glucose as glycogen in the hepatocyte cells of the liver, and deactivates glycogen phosphorylase, which breaks glycogen down into glucose.
Glucogon works by reversing the effects of insulin. It forces the liver to release glucose into the bloodstream. Glucogon is released by the alpha cells in the pancreas when blood glucose levels are too low. When glucogon arrives in the liver, it phosphorylates glycogen synthase and glycogen phosphorylase, reversing what insulin did to them. This activates glucogen phosphorylase, which breaks down the glycogen that's stored in the liver into glucose. It also deactivates glycogen synthase, which stores glucose as glycogen when active.
Glucogon also activates the breakdown of triglycerides (fats) in adipose cells by phosphorylating triacyglyceral lipase. The fatty acid products of this breakdown are transported to the liver (and most other cells in the body), where they can be used for energy.
When fat cells accumulate large amounts of fat, they need to be able to tell the brain to stop sending them more glucose for storage. They do this through the creation of leptin. The production of this protein in white fat cells increases in proportion to the amount of fat in the cells. The small leptin molecules diffuse out of the fat cells and into the bloodstream. They then bind to leptin receptors on the surfaces of brain cells in the hypothalamus. This stimulates activity in the brain that reduces appetite, and therefore glucose intake.
Leptin may not seem to be an effective regulator of fat storage, since so many of us are overweight. The situation would be much worse, though, if we were always hungry. The hunger we are talking about here is triggered by the depletion of fat in the cells, not the hunger we experience between meals. Most people in affluent communities never experience this level of hunger. Without any leptin circulating in our system, we would be experiencing "starvation" all of the time. Mice that are unable to produce leptin are not able to stop eating, and become grossly obese. So even though we sometimes reach for that extra doughnut when we aren't very hungry, leptin is more effective than we might think.
On the Post Calvin Cycle page we saw how plants use energy to create and store carbo-hydrates in the foods we eat. On this page we follow the digestion of carbohydrates from the time they enter our mouth to the point where the glucose molecules cross the cell walls to take part in cellular respiration.
This page is one of several that examine how carbohydrates are created and consumed. Links to the other pages can be found on the main carbohydrates page or the site map.
Maintaining balance in molecular biology is so important it's been given a special name: Homeostasis. All of the nutrients we depend on must be available in the proper amounts or many of the processes that keep us alive will start to shut down. Maintaining proper levels of glucose in the bloodstream is no exception.

On the left side of this page we've seen how things work when the pancreas and liver are able to successfully regulate glucose levels in the blood. It's a complicated process, and many things can go wrong. In the sidebars below we look at some of the challenges the body must deal with when trying to maintain blood-sugar homeostasis, and the problems that result when it's unable to do so.
The glycemic index measures how quickly blood-sugar levels rise when one gram of digestible (non-fiber) carbohydrate in a given food is consumed. One gram of pure glucose is the standard, with it's glycemic index set at one hundred.
The carbohydrate content in all other foods has a lower glycemic index number than pure glucose because the carbohydrates have to be broken down before they are absorbed, or their absorption is slowed down by the presence of other molecules. Starch breaks down more slowly than sucrose, and glucose doesn't have to be broken down at all. Fiber and non-carbohydrate molecules can slow down absorption by getting in the way.
The reason the glycemic index is important is because too much glucose dumped into the blood too quickly produces an insulin spike. It's better if the carbohydrates are broken down and absorbed into the bloodstream over an extended period of time.

This whole grain bread has a lower glycemic index than it's white bread counterpart. This is because whole grain bread contains more fiber (cellulose) than white bread. The fiber slows down the absorption of the digestible carbohydrates.
It's important to note that the glycemic index doesn't tell you how much carbohydrate is in a serving of food, only how fast a gram of it will enter the bloodstream. A more useful measure of the effect a food will have on the magnitude of a potential insulin spike is the glycemic load. The glycemic load multiplies the glycemic index of a food by the number of grams of digestible carbohydrate that are in a serving of that food.
Diabetes is a disorder that's defined by the inability of our bodies to sustain a healthy balance in blood-sugar levels. Maintaining homeostasis in a system as complicated as the one described on the left side of this page can be difficult, and many things can go wrong. While there are many contributing factors to the development of diabetes, they can be divided into two main types.
Type 1 diabetes is caused by damaged beta cells in the pancreas, which limits the amount of insulin a person can produce. It's a rare condition compared to type 2 diabetes.
Type 2 diabetes is at epidemic proportions. It's not caused by a lack of insulin, but by the body's inability to respond to the insulin in an effective manner. This condition is generally called insulin resistance, and can be caused by a number of things. I've listed a few of the possibilities below.
1. There may be too few insulin receptors, or the receptors might not bind to insulin like they should.
2. Conditions inside the cell might not allow for reactions that create GLUT4 openings for the passage of glucose into the cell.
3. It's also possible that the insulin isn't able to dephosphorylate the enzymes in the liver's hepatocyte cells that control glucose release from the liver.
It's a complicated system, and much can go wrong. Even less certain are the biochemical reactions that create this resistance, because the effects of these reactions develop over time. On a behavioral level a healthy diet and exercise seem to decrease insulin resistance, while obesity increases it. Genetics may also play a role.
People with type one diabetes need regular injections of insulin because their pancreas cannot produce it. Many type two diabetics also use insulin injections to compensate for the effects of insulin resistance. They monitor their blood-sugar levels and use more insulin as needed.